There are many factors that can lead to a dental implant failing, even after initially showing signs of successful embedding in the jaw bone.
These factors are taken into consideration when patients considering having dental implants visit their dentist. The patients go through an assessment process to see whether they are suited for this treatment.
With advances in implant surgery, bone grafting and aftercare, patients that could not have implants in the past due to some biological and health limitations, are now able to enjoy this great tooth replacement option.
There are many factors and risks that can determine the success of implant treatment.
These factors can have an effect before, during or after the implant surgery.
Bisphosphonates (Alendronic Acid)
Patients taking Bisphosphonates for Osteoporosis are at higher risk when it comes to implant treatment. Bisphosphonates have shown very good results against Osteoporosis, slowing down bone loss in general by altering the bone remodelling process that constantly takes place in the bones of the body. But the medical and dental community realised that Bisphosphonates has severe side effects when it comes to the healing of the jaw bone after tooth extractions and other surgical procedures in the jaw area such as implant placements. Therefore, patients who have been taking the medication have to be carefully assessed. The dentist may advise the patient to stop the medication for a period of time before undergoing the implant surgery. Intravenous injections of Bisphosphonates can have a long lasting effect, even years after the last injection has been administered, therefore care should be taken when planning the timing of surgery.
Smoking
Chemicals in tobacco products restrict the flow of blood to the gums by closing the small blood vessels (capillaries). This makes it more difficult for the body to fight potential infections and to heal after surgery in the mouth. Therefore it is recommended to quit smoking a few weeks before the implant surgery to allow the gum to recover and go back to its healthy state. It is also advised not to smoke after the implant surgery, or at least for a few weeks afterwards to allow the healing of the surgery site.
Gum disease:
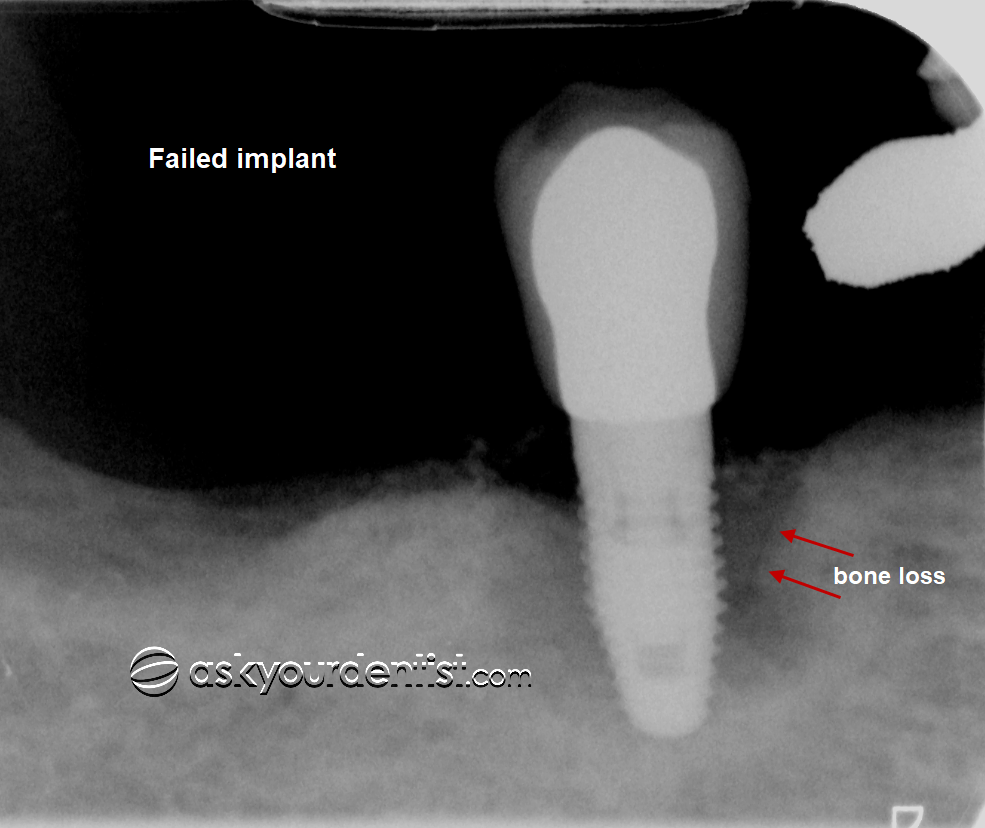
A certain percentage of the population have a genetic predisposition to gum disease. This means that their gums are more susceptible to infections with bone loss as a result of this.
Studies have shown that even patients who have had all their teeth out and replaced them with implants, can still develop similar infections around the implants.
Diabetes:
Patients with Diabetes take a longer time to heal after surgery. This could have an adverse effect on the implant surgery.
- Bone quality and bone volume in the implant site:
Bone quality varies in different locations of the jaw, and also between the upper and the lower jaw. Porous bone is less favourable than compact bone. The bone is more compact in the lower jaw compared to the upper jaw. Bone volume plays a big role in determining the success of the implant outcome.
Early loading of the implant screw:
The dental implant should be allowed to heal (osseo-integrate) without it being disturbed by loading forces. It usually takes 10 to 14 weeks for an implant to heal properly before an implant crown (the tooth) is placed on it. If the implant is exposed to pressure before healing properly, this may cause it to fail. Dental companies and dental schools are investing a lot of time and money to find ways to make the healing process quicker.
Poor oral hygiene:
It is very important to have good oral hygiene and good cleaning routines after the implant treatment.
The implant surface behaves in a similar way to a normal tooth and will get infected by bacteria and will develop bone loss if not cleaned properly.
The patient is encouraged to see a dental hygienist on a regular basis to ensure the site of the implant is properly cleaned to prevent bone loss (peri-implantitis) around the implant.
Allergies:
Although allergy to dental implants is very rare, there have been reported cases of hypersensitivity to Titanium. This can be due to other sensitising agents such as Nickel, Chrome and Cobalt in the metal that have worked their way in during the production process of the implant screw. Titanium is bio-compatible and is not rejected by the body compared with other metals, but patients who are more sensitive to other metals should be tested for titanium sensitivity/allergy before any implant treatment.
- Other factors that may affect implant treatment: patients undergoing chemotherapy and patients undergoing Antithrombotic treatment with an increased risk of bleeding.
To find out more and to chat one-to-one with a qualified dentist, please go to the chat box on the right.